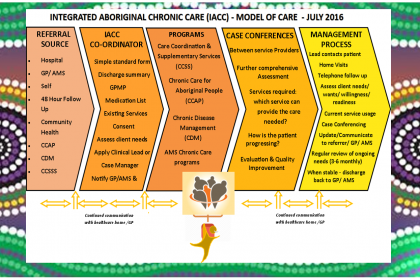
Since its first referral back in May 2017 the Integrated Aboriginal Chronic Care (IACC) program has continued to improve the patient journey between all Aboriginal-specific chronic care services in Northern NSW via its unique single point of assessment system. Since its inception IACC has received over 165 referrals.
The “No Wrong Door” referral system is the linch pin of the IACC program which has seen improved outcomes for Aboriginal Chronic Care patients in Northern NSW. IACC empowers its clients by ensuring the right care, in the right place at the right time – a fundamental element of Integrated Care.
IACC empowers its clients by ensuring the right care,
in the right place at the right time
IACC maintains these strong partnerships by holding regular meetings, altogether 54 team care conferences and 4 IACC team workshops have been held. At the workshops the team participates in sessions aimed at improving seamless integrated care between Aboriginal Chronic Care Service networks and the referral pathways of the IACC partners.
IACC continuously evolves its shared care planning through partnerships, communication, integration, trust, awareness and accountability. At the team workshop IACC focuses on what is working and what is not, allowing ownership and change to improve holistic care. Issues addressed include:
- Improvement of external service delays and contact issues
- Improving patient contact
- Transient and cross border clients’ care management
- Managing appointments and compliance and of course improving patient, family and Community interactions
IACC is approaching the evaluation phase of the program and the team lead by Ragina Rogers, IACC Coordinator is excited to display the success of our Shared Service.

IACC Key Features:
- Single point of assessment to access all Aboriginal specific chronic disease management programs
- Comprehensive assessment of patient needs and onward referral to most appropriate services regardless of which service receives the referral
- Case management, care co-ordination, self-care support and healthy lifestyle programs through service collaboration.
- Routine coordinated case conferencing and ongoing assessment of needs.
- Reduced duplication between similar services ensuring patients have co-ordinated access to all appropriate services.
- Cooperation between primary, secondary and tertiary health services.
IACC Impacts and Benefits:
For Patients
- One clearly designated case manager
- Seamless service delivery
- Entry into services and programs in a timely manner
- Ease and improved navigation of chronic care programs /health
- Comprehensive and multidisciplinary assessment and management of chronic conditions
- Improved communication lines between services to co-ordinate care
- Better health outcomes
- Fewer unplanned admissions to hospital
- Access to all appropriate services at the appropriate time
- More opportunity to access and improved support for all types of chronic care services
For Services
- Through these partnerships, the network of services will provide support to ensure patients ‘don’t fall through the cracks’
- The teams’ capacity will enable continuity of care, even if individual case managers are unavailable
- More complete, internal and external communication between all parties throughout the patient health journey
- Referral processes to service won’t change but easier access to more services
- No extra staff required but increased availability to other services
- Comprehensive approach to individual patient care
- Improved relationships between services
- Improved relationships with general practice and external referrers to the program
- Cost effective systems both administration and support
- Improved and more effective management of patient’s health care needs
- Financial benefits from coordinated care (via MBS)
For Providers
- One contact number for all services
- Clear and concise referral system for all services
- Improved communication internal and external
- New system supports timely referrals and responses regarding patient
- A collaborative approach to each client rather than a splintered approach where each health professional and program do not connect
- Avoidance of duplication, awareness by ‘health team’ of who, what, why, how and where client care is being delivered
- Regular case conferencing with the health team and established feedback mechanism
Here are some of the hard working staff who are working better together alongside LHD staff such as the Chronic Disease Management Service (CDM) and through collaboration are contributing to the success of the IACC program:

