
What are we trying to do?
To understand and improve the patient journey between all Aboriginal specific chronic care services in Northern NSW geographical areas, between Grafton and Tweed Heads, to develop and implement Integrated Aboriginal Chronic Care (IACC) with partner services.
Key Issues and Causes
- Several similar services exist for Aboriginal chronic care clients across LHD footprint within different organisations
- There were various methods to access similar services ie. intake process/ criteria/ level of care/ capacity
- Poor communication between services all accessing the same client group
- Inequity of access to services at all levels of care
- Some clients were receiving all services, some were receiving none
- Limited awareness of what other services offered
Background
A partnership between the Northern NSW Local Health District, North Coast Primary Health Network, local Aboriginal Medical Service’s and General Practice has been developed to streamline and simplify access to all Aboriginal specific chronic disease services and rehabilitation programs within the Northern NSW region.
Following thorough workshopping and surveying the partnering organisations determined that similar services were provided across all organisations. There was an overwhelming need to improve communication between Aboriginal specific chronic care services, to reduce duplication, ensure all patients have equal access to services needed, and increase the understanding amongst staff regarding level/ type of care provided by other services.
An additional core element of this initiative is to improve referral to, commencement and completion of healthy lifestyle (chronic disease rehabilitation) programs including the development of Aboriginal specific home based lifestyle programs.
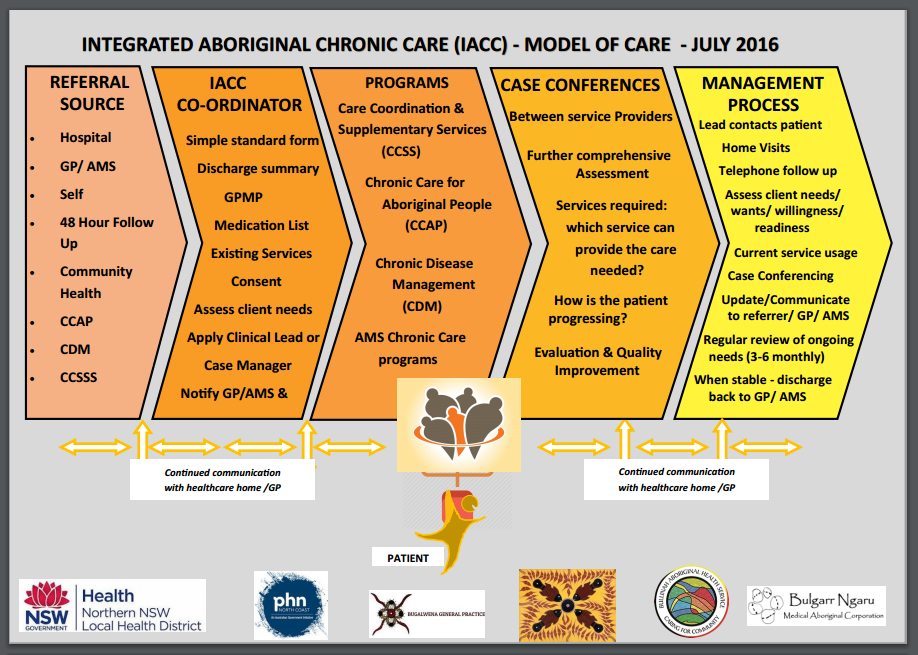
Key features of Integrated Aboriginal Care include:
- Single point of assessment to access all Aboriginal specific chronic disease management programs
- Comprehensive assessment of patient needs and onward referral to most appropriate services regardless of which service receives the referral
- Provision of case management, care co-ordination, self-care support and healthy lifestyle programs through service collaboration
- Routine coordinated case conferencing and ongoing assessment of needs
- Reduced duplication between similar services ensuring patients have co-ordinated access to all appropriate services
- Cooperation between primary, secondary and tertiary health services.
How Will it Work?
What are the Impacts and Benefits?
For Patients
- One clearly designated case manager
- Seamless service delivery
- Entry into services and programs in a timely manner
- Ease and improved navigation of chronic care programs /health
- Comprehensive and multidisciplinary assessment and management of chronic conditions
- Improved communication lines between services to co-ordinate care
- Better health outcomes
- Less unplanned admissions to hospital
- Access to all appropriate services at the appropriate time
- More opportunity to access and improved support for all types of chronic care services
For Services
- Through these partnerships, the network of services will provide support to ensure patients ‘don’t fall through the cracks’
- The teams’ capacity will enable continuity of care, even if individual case managers are unavailable
- More complete, internal and external communication between all parties throughout the patient health journey
- Referral processes to service won’t change but easier access to more services
- No extra staff required but increased availability to other services
- Comprehensive approach to individual patient care
- Improved relationships between services
- Improved relationships with general practice and external referrers to the program
- Cost effective systems both administration and support
- Improved and more effective management of patient’s health care needs
- Financial benefits from coordinated care (via MBS)
For Providers
- One contact number for all services
- Clear and concise referral system for all services
- Improved communication internal and external
- New system supports timely referrals and responses regarding patient
- A collaborative approach to each client rather than a splintered approach where each health professional and program do not connect
- Avoidance of duplication, awareness by ‘health team’ of who, what, why, how and where client care is being delivered
- Regular case conferencing with the health team and established feedback mechanisms

You must be logged in to post a comment.