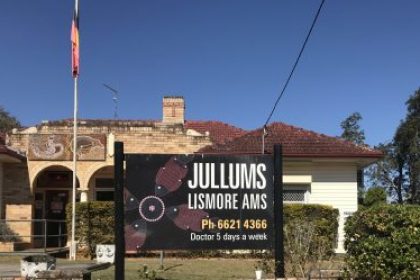
Clinicians from Jullums, Lismore’s Aboriginal Medical Service and the NNSWLHD Community Mental Health and Drug and Alcohol are meeting monthly to discuss mutual clients in an exciting new integrated care pilot. The “Health Partnership” is a first for the Northern Rivers and aims to trial an innovation that integrates primary and tertiary services for Aboriginal patients with severe mental health illness, with a specific focus to address physical health care.
The trial aims to increase the rates of metabolic monitoring, increase safety in prescribing and most importantly improve the experience for people using the services.
Health Partnerships demonstrates the NSW Health Guideline for the Physical Health Care of Mental Health Consumers with appropriate linkages with other health care providers; the building of stronger partnerships with key stakeholders; and establishing minimum expectations for the physical health care of consumers.
The Health Partnership was initially formed as part of the Integrated Care Collaborative (ICC); a local partnership between the NNSWLHD, North Coast Primary Health Network, Aboriginal Medical Services and the NSW Ambulance. The implementation of the ICC provided a mechanism for a multi-disciplinary team from across the system to engage and have license to test new ideas by implementing small changes and measuring the effects.
Health Partnerships was initiated by Sandy O’Brien, (Integrated Care NNSWLHD), Jacqui Laurie (Aboriginal Support NNSWLHD), Vickie Williams (Practice Manager Jullums) Dr Peter Silberberg, Dr Andrew Binns (Jullums), Kate Salisbury (NUM Riverlands OTP).

From Left to right: Dr Andrew Binns; Sandy O’Brien; Jacqui Laurie; Kate Salisbury; and Vickie Williams
How does the CMH and Jullums Health Partnership Work?
Initially Jacqui Laurie and Dr Peter Silberberg collaborated to identify mutual patients. The Health Partnership has since identified 5 patients with complex comorbidities that would benefit from this trial.
The following is the agreed-upon workflow which is being utilised and is consistent with all services.

E-faxing from the NNSWLHD is being utilised to streamline communication to Jullums. . The use of eFax also bypasses administrative intervention. Each team shares the agreed health information.
Overcoming Challenges as a Team:
Communication between the LHD and Jullums remains an ongoing work in progress. Increase in communication has been helped by
Regular networking that eases communication with difficult conversations and challenging clients
Including other members of the patients care team as required such as Community nurses and peer support.
Admission and Discharge Notifications (ADNs). Jullums GP will receive notification for any unplanned admissions and/or discharge from a NNSWLHD hospital.
Discharge Summaries from Riverlands Detox Unit are now available electronically via the e-health portal and MHR.
Solutions in Planning:
The use of My Health Record in particular for pathology results and accessing Specialists’ letters will be explored further and incorporated into the current model.
Case Conferencing involving the patient and/or carer. This patient-centred approach will allow the patient to contribute and consent to their own treatment.
Expanded MDT case conferencing.
eMR scanning which should allow information received from a GP to be uploaded in eMR is on the NNSWLHD Exec agenda with a brief submitted for consideration
The Future of Health Partnerships:
The North Coast Primary Health Network is working collaboratively with local GPs and the NNSW LHD to develop a mental health trial in Lismore. Lessons learnt as part of the CMH and Jullums Health Partnership will identify what can be replicated. Discussions have begun to identify scalability of the trial.
